
Hasan Hazim Alsararatee
Acute Medicine/ SDEC, Northampton General Hospital NHS Trust, Northampton, Northamptonshire, UK.
*Corresponding Author: Hasan Hazim Alsararatee, Acute Medicine/ SDEC, Northampton General Hospital NHS Trust, Northampton, Northamptonshire, UK.
Received Date: January 17, 2024
Accepted Date: January 23, 2024
Published Date: February 14, 2024
Citation: Hasan Hazim Alsararatee. (2024) “Atypical Presentation of Pulmonary Embolism Masquerading as Abdominal Pain.”, International Journal of Medical Case Reports and Medical Research, 2(1); DOI: 10.61148/2994-6905/IJMCRMR/022.
Copyright: © 2024. Hasan Hazim Alsararatee. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This case report presents a rare manifestation of pulmonary embolism (PE) with atypical abdominal pain, highlighting the diagnostic challenges encountered. A female patient in her early eighties initially presented with left upper abdominal pain, initially treated for Urinary Tract Infection (UTI), and later accurately diagnosed with PE through Computed Tomography Pulmonary Angiography (CTPA). Various mechanisms of abdominal pain in PE are discussed, including right-sided heart failure-induced hepatic congestion and diaphragmatic irritation from pulmonary lobe infarction. Despite dyspnea and chest pain being more common, abdominal pain is documented in 6.7% of cases. This case underscores the importance of considering PE in the differential diagnosis of abdominal pain, particularly in the elderly population, to prevent potentially fatal consequences.
Background:
PE is one of the most common presentations to the Emergency Department (ED) and often is misdiagnosed leading to high mortality and morbidity [1]. The missed diagnosis rate for PE reportedly exceeds 70%, with only 7% of deceased PE patients diagnosed before death [2]. In contrast, while the hospitalization mortality rate for PE ranges from 2.5% to 10%, the mortality rate for those with a missed diagnosis is typically acknowledged to be 30% [3]. However, some literature highlights that the actual prevalence of PE remains uncertain. Inaccurate estimates of PE prevalence may, to some extent, arise from the under-recognition of atypical presentations of this condition [4]. Abdominal pain emerges as an atypical manifestation of PE, with a notable association highlighted in a comprehensive 2011 study where 10.7% of 1880 diagnosed PE patients reported upper abdominal pain [5]. Additionally, rare instances of resolved abdominal pain following anticoagulant treatment have been reported as part of these atypical presentations [6]. Thus, clinicians should uphold a systemic approach and recognise the imperative need to contemplate the potentiality of a fatal diagnosis, particularly in cases characterised by unexplained abdominal pain. Clinical suspicion and a thorough diagnostic approach are crucial in such cases, emphasising the need for prompt evaluation and appropriate imaging to ensure timely diagnosis and management.
Case presentation:
81-year-old-female was referred from ED to SDEC due to the sudden onset of left sharp abdominal pain persisting for 72 hours. The pain is not radiated, no reliving or exaggerating factors, not associated with other symptoms. It was 6/10 on pain score. Her medical history encompassing hypertension and hypercholesterolemia, she denied any dysuria or haematuria. No recent trauma or falls, or any association with COVID-19 or COVID-19 vaccinations. She states that was opening her bowel and bladder normally. Additionally, there was no significant family history of respiratory or cardiovascular diseases. Initial assessments by surgical and urology teams concluded that acute surgical intervention was unnecessary, and an abdominal ultrasound revealed no abnormalities. However, a urine culture indicated White Blood Cells (WBC) >200 cells/mm3 and urinalysis (Dipstick) shows leukocytes of ++, and Nitrates of ++, prompting treatment for a urinary tract infection (UTI). Her observations include blood pressure measured 132/80 mmHg, and the heart rate was 75 beats per minute. Temperature: 36.2°C, respiratory rate: 18 bpm and saturation of 98%. Also, she had a PaO2 of 97 mmHg. She was a well-nourished female, slightly uncomfortable in bed, without jugular venous distention or calf tenderness/erythema. There were no murmurs or rubs but fine crackles in the left lower base. The abdomen was tender in the left upper quadrant, with no signs of rebound or guarding. Murphy’s sign was negative. No lower limbs pitting oedema. The Wells score indicated a moderate risk (3), promoting the decision to measure the D-dimer level which was found to be 2210 ng/m. This result led to a referral to Same Day Emergency Care (SDEC) for a comprehensive review, considering the possibility of PE.
Blood investigations revealed a C-Reactive Protein CRP level of 114 mg/L (normal range: 0 - 5) and a WBC of 14.0 x 10^9/L (normal range: 4.0 - 10.0). Troponin T levels were below 13 ng/L, and urea and electrolytes remained within normal limits. The D-dimer test indicated elevated levels at 2210 ng/m. A COVID-19 test yielded negative results, and blood cultures along with sputum gram stain with culture returned negative results. The electrocardiogram (ECG) displayed a normal sinus rhythm (Figure 1).

Figure 1: 12 leads ECG, normal sinus rhythm
A CXR revealed minimal left-sided pleural effusion, potentially suggestive of infection or infarction (Figure 2). Due to observed pleural effusion on the CXR and elevated D-dimer levels, a CTPA was performed, revealing multiple filling defects in the left lower pulmonary artery and pleural effusion in the right lower lobe, accompanied by mild right pleural effusion, suggestive of an infective or inflammatory aetiology (Figures 3). The patient was subsequently started on therapeutic anticoagulant therapy. However, she developed a dry cough and ALT is slightly rising with normal Bilirubin and ALP. Abdominal ultrasound was performed to rule out portal vein thrombus which was negative. CT abdominal was done which was no acute pathology was identified. A repeat CXR shows left left-sided pleural effusion is getting bigger slightly (Figure 4) compared to the initial CXR (Figure 2).

Figure 2: minimal left-sided pleural effusion.
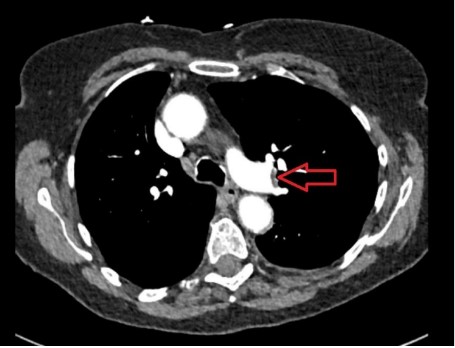
Figure 3: CTPA filling defects in the left lower pulmonary artery and pleural effusion in the left lower pulmonary lobe.
Treatment:
She was treated for UTI with oral Fosfomycin 3 g and treated for unprovoked PE with Rivaroxaban 15 mg BD for 21 days followed by 20 mg OD for 4 months. The patient was covered with oral Co-amoxiclav 625 mg TDS for 5 days for community-acquired pneumonia as well since developing the cough with high inflammatory markers. After five days, the cough and abdominal pain are completely resolved.
Outcome and follow-up:
After five days of completing the above antibiotics, the cough and abdominal pain are completely resolved. She is doing well on four weeks follow-up.
Discussion:
The clinical manifestations of PE are often nonspecific, posing challenges to diagnosis. Notably, acute surgical abdomen is not commonly listed as presenting features of PE. The typical presentation of PE encompasses dyspnoea (80%), chest pain (52%), cough (20%), haemoptysis (11%), and syncope (19%) [7]. Conversely, the atypical presentation includes abdominal pain, high fever, new-onset atrial fibrillation, and disseminated intravascular coagulation [7]. When abdominal pain is present in the context of PE, it is usually accompanied by other typical PE symptoms, highlighting the importance of recognizing the diverse clinical manifestations of this condition. However, this was not the case in our case study as the patient has left upper quadrant and flank pain.
When patients present with abdominal pain, healthcare professionals prioritize abdominal pathologies, considering myocardial infarction or pleurisy, rarely considering pulmonary embolism [8]. In this case report, the patient initially attended with abdominal pain without typical PE symptoms such as pleuritic chest pain or shortness of breath, was initially misdiagnosed with UTI. In our case report, it was only after observing an elevated D-dimer level and conducting a comprehensive examination the suspicion of PE emerged.
A variety of potential mechanisms that contribute to abdominal pain associated with PE are explained. One perspective suggests that PE can induce abdominal pain, attributing the pain to hepatic congestion resulting from right-sided heart failure induced by PE [9]. Previous literature supports that this explanation is considered a primary cause of PE-related abdominal pain [10]. However, this was not the case with our case report as the patient did not have RV dilation. Increased right ventricle pressure leads to paradoxical embolism and reduced blood supply to abdominal organs [10]. Another theory suggests that increasing the blood viscosity, alongside low oxygen levels, may generate small emboli causing focal necrosis in abdominal organs which leads to abdominal pain [11]. However, another theory explains that pulmonary hypertension associated with PE is implicated in abdominal lymphedema and hepatobiliary portal infiltration [12]. Additionally, previous literature points out that abdominal pain may be referred from the chest and causing chest pain, potentially arising from pulmonary hypertension or thrombus stimulation of sensory nerve endings in blood vessel walls, or lateral diaphragmatic stimulation [12]. Alternatively, abdominal pain may result from diaphragmatic irritation from the pulmonary lobe infarction. In our case report, the abdominal pain might be from the infarction of pneumonia [13].
In conclusion, this case highlights a significant example of PE that could have been easily missed without a heightened level of suspicion. It emphasizes the critical need for a comprehensive and systematic approach when investigating nonspecific symptoms, emphasizing that abdominal pain can serve as the primary and sole presenting complaint in PE, leading to a diagnosis that can be lifesaving. Recognizing abdominal and flank pain as potential presenting symptoms of PE is essential to prevent diagnostic delays. It underscores the imperative for clinicians to remain vigilant, as a missed diagnosis of this potentially devastating condition carries significant consequences.
Learning points/ take-home messages:
List of Abbreviations:
PE: Pulmonary Embolism
ED: Emergency Department
CTPA: Computed Tomography Pulmonary Angiography
WBC: White Blood Cells
UTI: Urinary Tract Infection
CRP: C-Reactive Protein
ECG: Electrocardiogram
USG: Ultrasound
ECHO: Echocardiography
Patients’ perspective:
The patient expresses heartfelt gratitude for the attentive care and the discovery of pulmonary embolism (PE) through the CT scan. She is genuinely thankful for the dedicated medical teams and the author for their commitment to her well-being.